Knee Arthroscopy
- Home
- / Knee arthroscopy
Knee Arthroscopy
Dr Rohan Bansal performs the least aggressive and most advanced techniques in arthroscopic and open knee surgery. Minimally invasive techniques and use of plasma membranes Rich in Factors (MPRGF) as a healing accelerator. Expert in anterior cruciate ligament reconstruction surgery, meniscal surgery and cartilage transplants: More than 1000 knees operated on.
INDICATIONS OF KNEE ARTHROSCOPY:
- Synovectomy
- Meniscus tear.
- Meniscal transplant.
- Cartilage transplantation and cartilaginous lesions.
- Anterior and posterior cruciate ligament rupture.
- Patellofemoral instability.
- Fractures.

MENISCUS
Your knee is the largest joint in your body and one of the most complex. Because you use it so much, you are vulnerable to injury. Because it is made up of so many parts, many different things can go wrong. Meniscus tears are among the most common knee injuries. Athletes, especially those who play contact sports, are at risk for meniscal tears. However, anyone at any age can tear a meniscus. When people talk about torn knee cartilage, they are usually referring to torn menisci.
ANATOMY
normal knee anatomy
Three bones come together to form your knee joint: the thigh bone (femur), the shinbone (tibia), and the ball joint (patella). Two wedge-shaped pieces of cartilage act as “shock absorbers” between your femur and tibia. These are called menisci. They are strong and elastic to help cushion the joint and keep it stable.
DESCRIPTION
Menisci tear in different ways. Tears are defined by their appearance and also by where the tear occurs in the meniscus. Common tears include longitudinal, parrot beak, flap, bucket handle, and mixed/complex. Sports-related meniscal tears often occur along with other knee injuries, such as anterior cruciate ligament tears.
CAUSE
Sudden tears of the menisci often occur during sports. Players can squat and twist the knee, causing a tear. Sometimes there is direct contact involved, for example a tackle in rugby. Regular movements that are made during work can cause injuries.
Older people are more likely to have degenerative meniscal tears. The cartilage weakens and wears away, thinning over time. Worn and aged fabric is more prone to tears. Just twisting hard when getting up from a chair could be enough of a tear if the menisci have weakened with age.
SYMPTOMS
You may feel a “pop” sound when a meniscus tears. Most people still walk with an injured knee. Many athletes continue to play with a tear. After 2 or 3 days, your knee will gradually become stiffer and more swollen.
THE MOST COMMON SYMPTOMS OF MENISCUS TEARS ARE
Pain
stiffness and inflammation
Immobilizing or locking your knee
The feeling that your knee is "collapsing"
You are not able to move your knee through its full range of motion.
Without treatment, a piece of the meniscus could become loose and migrate into the joint. This can cause your knee to buckle, pop, or lock.
MEDICAL EXAM
PHYSICAL EXAMINATION AND PATIENT HISTORY
After discussing your medical history and symptoms, the doctor will examine your knee. He will check if there is pain on pressure in the joint line where the meniscus is located. This is often a sign of a tear.
One of the main tests for meniscal tears is the McMurray test. Your doctor will flex your knee, then bring it to a straight position and rotate it. This puts stress on a torn meniscus. If you have a meniscus tear, this movement will cause a ‘click’ sound. Your knee will ‘click’ each time your doctor does the test.
IMAGING EXAMS
Other knee problems cause similar symptoms, so your doctor may order imaging tests to help confirm the diagnosis. X-rays (X-rays): Although X-rays do not show meniscal tears, they can show other causes of knee pain, such as osteoarthritis. Magnetic resonance imaging (MRI): This test can create better images of the soft tissues of your knee joint.
TREATMENT
How your orthopedic surgeon will treat your tear will depend on the type of tear you have, its size, and its location.
The outer third of a meniscus has a large blood supply. A tear in this “red” area may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this type of tear. In contrast, the inner two-thirds of the meniscus lack a blood supply. Without blood nutrients, tears in this “white” area cannot heal. These complex tears often occur in thin, worn cartilage. Because the pieces cannot be reattached to regenerate, tears in this area are usually surgically trimmed.
In addition to the type of tear you have, your age, activity level, and any related injuries will all influence your treatment plan.
NON-SURGICAL TREATMENT
If your tear is small and at the outer edge of the meniscus, it may not require surgical repair. As long as your symptoms don’t persist and your knee is stable, non-surgical treatment may be all you need.
RICE: The RICE protocol is effective for most sports-related injuries. RICE is an acronym that stands for R=Rest, I=Ice, C=Compression and E=Elevation.
- R=Rest. Take a break from the activity that caused the injury. Your doctor may recommend that you use crutches to take weight off your leg.
- I=Ice. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly to the skin.
- C=Compression. To prevent further swelling and blood loss, wear an elastic compression bandage.
- E=Elevation. To reduce swelling, lean back when you rest and raise your leg above the level of your heart.
Non-steroidal anti-inflammatory drugs. Medicines like aspirin and ibuprofen reduce pain and inflammation.
SURGICAL TREATMENT
If symptoms persist with nonsurgical treatment, your doctor might suggest arthroscopic surgery.
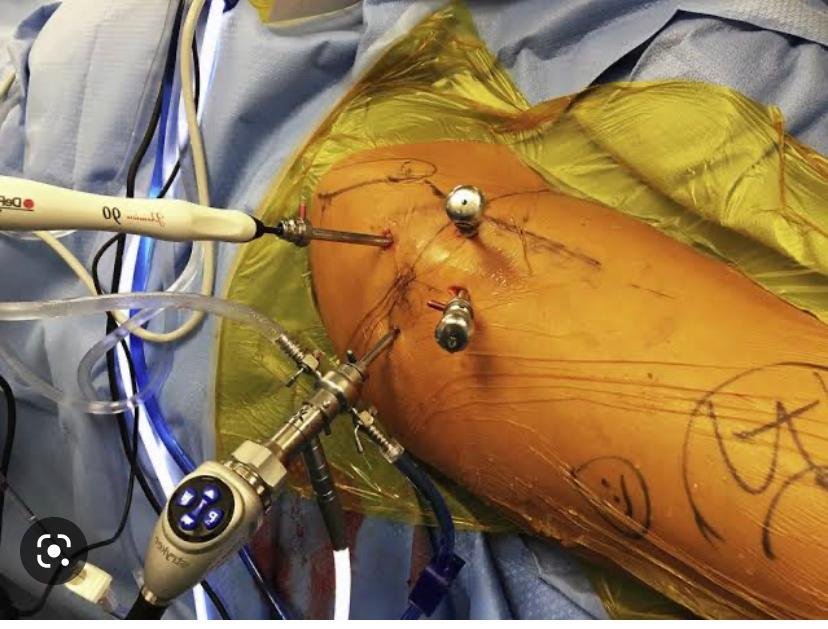
Procedure: Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, a miniature camera is inserted through a small incision. Arthroscopy gives a clear view of the inside of the knee. Your orthopedic surgeon inserts miniature surgical instruments through other small incisions to cut down or repair the tear.
Knee Arthroscopy
Meniscus repair
Rehabilitation:
After surgery, your doctor may put your knee in a cast or immobilizer to keep it from moving. When the initial healing is complete, your doctor will order rehabilitation exercises. Regular exercise is necessary to restore mobility and strength in your knee. You will start with exercises to improve range of motion. Strengthening exercises will gradually be added to your rehabilitation plan. Most rehabilitation can be done at home, although your doctor may recommend physical therapy.
RECOVERY
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
ACL Tears
One of the most common knee injuries is a sprain or tear of the anterior cruciate ligament (ACL). Athletes who participate in high-demand sports like soccer, football, and basketball are more likely to injure their ACLs. If you have injured an ACL, you may need surgery to restore full function of your knee. This will depend on several factors, such as the severity of the injury and your activity level.
ANATOMY
Normal knee anatomy, front view Three bones join to form your knee joint: the thigh bone (femur), shin bone (tibia), and patella. The patella is located on the anterior face of the joint to provide some protection. Bones are connected to other bones by ligaments. There are four primary ligaments in your knee. These act like strong ropes to hold the bones together and keep your knee stable.
COLLATERAL LIGAMENTS
These are located on the sides of your knee. The medial collateral ligament is on the inner surface and the lateral collateral ligament is on the outer surface of the joint. These control the sideways movement of your knee and protect by preventing unusual movement.
CRUCIATE LIGAMENTS
These are located on the inside of your knee joint. They cross each other in an “X” shape, with the anterior cruciate ligament in front and the posterior cruciate ligament behind. The cruciate ligaments control the movement of your knee back and forth.
The anterior cruciate ligament runs diagonally through the middle of the knee. It prevents the tibia from slipping out of position, which would leave it in front of the femur, and also provides rotational stability to the knee.
DESCRIPTION
About half of all anterior cruciate ligament injuries occur with damage to other structures in the knee, such as the articular cartilage, meniscus, or other ligaments. Injured ligaments are considered “sprains” and are graded based on a scale of severity.
Grade 1 sprains: The ligament is slightly damaged in a grade 1 sprain. It has been slightly stretched, but is still able to help keep the knee joint stable.
Grade 2 sprains : A grade 2 sprain stretches the ligament to the point where it becomes loose. It is often called a partial ligament tear.
Grade 3 Sprains: This type of sprain is more commonly called a complete ligament tear. The ligament has been divided into two pieces and the knee joint is unstable.
Partial tears of the anterior cruciate ligament are rare; most ACL injuries are complete or near-complete tears.
CAUSE
The anterior cruciate ligament can be injured in several ways:
- Quickly changing direction.
- Stopping suddenly.
- Slowing down while running.
- Landing incorrectly from a jump.
- By direct contact or collision, such as a football tackle.
Several studies have shown that female athletes have a higher incidence of ACL injuries than male athletes in certain sports. It has been suggested that it is due to differences in fitness, muscle strength, and neuromuscular control. Other suggested causes include differences in pelvic and lower extremity (leg) alignment, increased slack in ligaments, and effects of estrogen on ligament properties.
SYMPTOMS
When you injure an ACL, you may hear a “crunch” and feel your knee give way, leaving you unsupported. Other typical symptoms include:
- Pain with inflammation. In the next 24 hours, your knee will swell. Without treatment, the swelling and pain may resolve on their own. However, if you try to return to sports, your knee will likely be unstable and you risk further damage to the cartilage that cushions your knee (meniscus).
- Loss of full range of motion.
- Pressure pain along the joint line.
- Discomfort when walking.
- rt.
MEDICAL EXAM
- Physical exam and patient history:During your first visit, your doctor will discuss your symptoms and medical history with you. During the physical exam, your doctor will check all of the structures in your injured knee and compare them to your uninjured knee. Most ligament injuries can be diagnosed with a complete physical exam of the knee.
- Imaging tests:Other tests that may help your doctor confirm your diagnosis include:
- X-rays (X-rays):Although they will not show any injury to your ACL, X-rays can show if the injury is associated with a broken bone.
- Magnetic resonance imaging (MRI):This test creates better images of soft tissues, such as the anterior cruciate ligament. But an MRI is usually not required to make the diagnosis of a torn ACL.
TREATMENT
- Treatment for an ACL tear will vary based on the individual needs of the patient. For example, the young athlete who performs agility sports will most likely require surgery to safely resume sports. The less active person, usually older, could return to a more sedentary lifestyle without surgery.
- NON-SURGICAL TREATMENT
- A torn ACL will not heal without surgery. But non-surgical treatment could be effective for patients who are elderly or have a very low activity level. If the overall stability of the knee is intact, your doctor may recommend simple non-surgical options.
- Braces/immobilizers:Your doctor may recommend a knee brace to protect your knee from instability. To further protect your knee, you may be given crutches to keep your leg from bearing weight.
- Physical therapy:As the swelling goes down, a careful rehabilitation program is started. Specific exercises will restore your knee function and strengthen the leg muscles that support the knee.
- SURGICAL TREATMENT
- Ligament Reconstruction:Most ACL tears cannot be reattached with sutures (stitches). To surgically repair the ACL and restore knee stability, the ligament must be reconstructed. Your doctor will replace your torn ligament with a tissue graft. This graft acts as a scaffold that will support the growth of the new ligament.
- Grafts can be obtained from various sources. They are often taken from the patella tendon, which runs between the kneecap and the tibia. The hamstrings on the back of the thigh are a common source of grafts. Sometimes a quadriceps tendon is used, which runs from the kneecap to the inside of the thigh. Finally, a cadaveric graft (allograft) can be used.
- There are advantages and disadvantages to all graft sources. You should discuss graft options with your orthopedic surgeon to help determine which is best for you.
- It takes time for the tissue to regrow, so it could take six months or more before an athlete can resume sports after surgery.
- Procedure:Surgery to reconstruct an ACL is done with an arthroscope using small incisions. Arthroscopic surgery is less invasive. The benefits of less invasive techniques include less pain from surgery, less hospital stay, and quicker recovery times.
- Unless ACL reconstruction is the treatment for a combined ligament injury, it usually isn’t done right away. This delay gives an opportunity for the swelling to resolve, and allows a return of movement before surgery. Performing an ACL reconstruction too early greatly increases the risk of arthrofibrosis, or scar formation in the joint, which would risk loss of motion in the knee.
REHABILITATION
- In any of the two cases, treatment with surgery or without surgery, rehabilitation plays a fundamental role in resuming daily activities. A physical therapy program will help you regain strength and movement in your knee. If you have surgery, physical therapy first focuses on restoring movement to the joint and surrounding muscles. This is followed by a strengthening program designed to protect the new ligament. This strengthening gradually increases the tension across the ligament. The final phase of rehabilitation aims at a functional return that adapts to the athlete’s spo
